Ulcerative Colitis
Receiving a diagnosis of a chronic illness can be frightening but educating yourself about your condition and effective symptom management will help you improve your overall wellness and health. Ulcerative colitis is one such condition That usually first appears in people aged 15 to 30 years. It is an autoimmune condition — this means that there is a problem with your immune system which is provoked due to physical or mental strain.
Overview
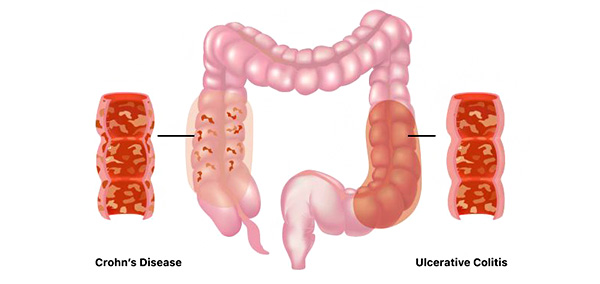
Ulcerative colitis is a kind of intestinal illness causing chronic inflammation of the cells lining your colon and rectum, also referred to as the large intestine. Usually, the rectum is where ulcerative colitis starts. This could result in bleeding sores known as ulcers producing blood pus and mucus, preventing your body from properly breaking down food. The small intestine is rarely affected. It rarely affects the entire big bowel at once. You can discover strategies to lessen the inflammation's impact on your day-to-day activities and take medication to reduce it.
We can provide the knowledge and tools you need to improve your mental and physical well-being. There are several subtypes of ulcerative colitis each named after the section of the colon affected,
Ulcerative proctitis: Only the rectum is affected
Proctosigmoiditis: affects the lower segment of the colon (sigmoid colon) and the rectum
Left-sided colitis: affecting the rectum sigmoid colon and descending colon up to the sharp bend near the spleen.
Total or pan-ulcerative colitis: which affects the entire colon
Causes
Genetic predisposition and environmental factors work together to create ulcerative colitis.
Diet genetics and environmental factors are risk factors for the illness.
Stress and diet can make the issue worse.
One study, for instance, discovered that consuming a lot of trans fats in many processed foods increases intestinal inflammation.
More common causes that have been related to IBD are,
Poor diet exposure to the harsh environment
Heredity and even specific medications.
Nonetheless, the illness is typically referred to as autoimmune.
Symptoms
Episodes of bloody diarrhea with variable lengths and intensities interspersed with periods without symptoms
An attack typically starts slowly with mild lower stomach cramps increasing urgency to urinate and mucus and blood in the stools.
Certain cases such as amebiasis and bacillary dysentery arise after an infection. The patient may have more than ten bowel movements a day frequently with excruciating cramps and uncomfortable rectal tenesmus without relief at night if the ulceration spreads proximally.
They may also experience looser stools. The feces are often almost totally composed of pus and blood and may be watery or mucus-containing.
The earliest symptoms of toxic or fulminant colitis include intense diarrhea that happens suddenly fever up to 40°C (104°F) stomach discomfort rebound tenderness and deep toxemia.
The stool may be normal or hard and dry when ulceration is limited to the rectosigmoid, although mucus discharges including red and white blood cells from the rectal cavity may accompany or happen in between bowel movements.
There are either no or little systemic signs.
Ayurvedic View
Grahani- due to following of nidanas (causes), like consumption of virudha ahara ( incompatible food), adhyashana (having food before digestion of previous food) etc, leads to agni mandhya (low digestion or metabolism) leads to prakopa (aggravation) of kapha dosha when person consumes guru (heavy), abhisyandi ahara (food that which blocks channel), this saama kapha (toxic causing) reaches grahani (duodenum-that which is responsible for metabolism and absorption) and blocks normal functioning of grahani, samana vayu, apana vayu, pachaka pitta (all responsible for food digestion and absorption) which leads to patient not having capacity to digest heavy food, with pitta dosha involvement there is bleeding due to formation of vruna (ulcer) in the pakvashaya (intestine ),this is ulcerative colitis. Ayurveda way of approach is to correct agni (metabolism) of jatara agni and dhatuva agni, bring dosha back to prakruta awastha (balance state-place, quality and normal functioning), improve proper functioning of grahani and reduce the disease symptoms, heal the ulcer by ayurvedic panchakarma treatment and internal medication.
Ayurveda Treatments
Abhyangam Anuvasana vasti Shirodhara Nabhi basti Lepanam.
Naturopathy Treatments
Diet therapy Enema Hip bath Packs Immersion bath Mud therapy Reflexology Chromotherapy Acupuncture Yoga therapy Cyclic meditation Mind sound resonance technique Pranayama Psychological counseling
Ulcerative Colitis
Treatment for
DISCLAIMER: Listed treatment details are only for information purposes. Treatments and duration may vary depending on numerous factors. Treatments for your condition may not be limited to this list.






















